The Internet of (Medical) Things is impacting healthcare positively. Continuous long term monitoring of patients’ health parameters allows healthcare professionals to intervene earlier and potentially save lives, patient time, and money through better utilization of healthcare resources. And yet many millions of people in the U.S. are living in poverty with limited access to healthcare and digital health technologies.
Limited access to typical digital health technologies and resources to send digital health information, e.g. smart devices or reliable access to the internet, among people of low socioeconomic status means that these people are being left behind. And on the clinic side, restricted budgets mean that clinics may have to forgo programs that could help improve or reduce the cost of chronic disease management.
-
In the U.S. chronic disease management makes up 75% of visits per year to free clinics
-
88 million Americans have pre-diabetes but 84% are not aware of it
-
108 million Americans have high blood pressure and only 24% have it under control
-
50 million in the U.S. live in poverty with limited access to healthcare
The team at Virginia Commonwealth University (VCU) of Amir Behdani, Briton Vanmaanen, and Emily Ko, have developed a solution using KNIME software and Amazon Web Services that will democratize digital health management. Amir, Briton, and Emily are Pharm.D. candidates at the Virginia Commonwealth University School of Pharmacy and founding members of Pharmacists for Digital Health, a student organization that strives to supplement their clinical training with the proficiency in digital health applications to better solve today’s healthcare challenges.
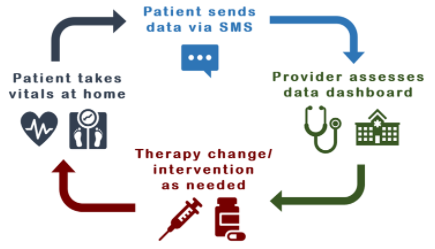
Their current research focus is based on a data pipeline to provide clinics with real-time patient reported data and democratizing healthcare by creating a platform accessible to all patients. Patients can send in updates on their health issues via text messaging for instance, removing the need for smartphones or stable internet connections.
The idea is to meet the patient wherever they are, with whatever tools they have available at home so they don't have to purchase any specialized equipment. Many already own a weight scale, glucose meters, etc, that are just not the particular models that integrate with the competitors' ecosystems.
A dashboard, based on a modular data pipeline, monitors blood pressure, blood glucose, exercise minutes - essentially any parameter relevant to the clinic’s practice.The clinic can track patient progress and intervene at an early stage, helping to improve health outcomes while keeping costs down for both patient and provider.
Let’s hear more about myDigitalARC directly from the team
Amir, Emily, and Briton talk to Stefan Helfrich, Academic Alliance Manager at KNIME.
Stefan: Did you have the idea(s) for the project before thinking about its implementation or did KNIME software and the possibilities it provides open up your mind to go for the project?
Emily: Our faculty and research mentor, Dr. Dayanjan Wijesinghe, showed us that clinical problems in today’s healthcare arena can sometimes have simple solutions - even solutions that beginners in data science can tackle as students in healthcare. KNIME Analytics Platform cleanly offered a way for us to tie the problem and solutions into a data pipeline, without any coding experience. The learning curve as total beginners was shortened by the intuitive logic between nodes, and the possibilities in KNIME for this project naturally opened wider as we grew more familiar with the platform.
Stefan: How much experience did you have in data science before starting the project?
Emily: No prior experience at all! I learned to see the world with my background in literature and chemistry, and seeing a world full of data for the first time was a wondrous experience.
Amir: I obtained a graduate certificate in health informatics and analytics before starting this project. I took some introductory courses in Python, SAS, R and SQL. I honestly wish I knew more about KNIME at the time. It was kind of challenging starting my journey in data science at the same time as my coding journey.
Stefan: Amir, you said you are actually a Python user. How do you find mixing Python - as a scripting language - together with KNIME - as a visual programming environment?
Amir: The combination of the two is something that I have been trying to learn through experience. I think they are both robust platforms with their advantages. I don’t think they are exclusive, and I believe they have some overlaps that can be used together to give the user more flexibility and make a more powerful tool combined for some advanced tasks.
Stefan: What is it about KNIME software that helps collaboration in your team?
Amir: I think the fact that no prior coding experience is needed is a great advantage. I personally had a hard time learning the basics of coding when I started working with Python. The user-friendly platform of KNIME gives more flexibility to the user to focus on their project outcomes rather than spending time learning the basics.
Our group consists of pharmacy students very interested in data science, digital health, etc. However, that does not mean that we want to become software engineers or computer scientists. The goal is to combine our clinical knowledge with powerful digital tools to improve patient outcomes. A platform like KNIME is a perfect tool to fulfill this goal because it allows the users to start working on their projects as soon as they know the basics, which is a lot easier and faster than code-based platforms.
Stefan: Emily, democratizing digital health is a very important topic for you: How does using KNIME support this?
Emily: Democratizing digital health starts with access to data on platforms that are accessible to all patients and clinics. By building our own data pipeline in KNIME and our own integrations with the clinic’s processes, we are cutting away the need to rely on third party services and thereby cutting the cost of our program for both patient and provider. KNIME Analytics Platform also gives us the ability to create multiple workflows for multiple disease states, giving clinics the freedom to collect patient data for multiple disease states and therapies without having to pay for multiple services.
As a side benefit, we are also learning how data can be used at the base. We often hear that technology is always changing, but the way tech is made and data is used at the core is more constant than the changing faces of tech. This basic understanding will give us the ability to continue to find efficiencies in the healthcare and technological gaps today and in the future.
Stefan: You have talked about KNIME connecting the dots. Could you explain what you mean by that?
Emily: Every element of our project in KNIME already exists individually, but we are connecting these disjointed dots into one package. We want to meet both patients and healthcare providers/clinics where they are, with the tools they already have. Many similar products do incorporate SMS messaging, but may not offer an affordable subscription plan for low-income patients. Or, they may give providers a means to track daily home blood glucose measurements, but only certain models of glucose monitors can be used to send data.
With KNIME, we were able to incorporate the most common denominators so that patients can be cared for no matter their socioeconomic background so that clinics can provide this care no matter their budget.
Our pipeline is also unique in that any parameter can be easily added, since we are building it ourselves in KNIME. Imagine a clinic that cares for patients with multiple chronic disease states. They’d need to purchase multiple packages or addons for each disease state to track, racking up the cost of providing this care, which may be transferred to the patient.
Stefan: Briton, assuming the project finds some funding: Where would you like to take the project?
Briton: Our goal is to empower as many patients as possible. Funding would allow us to expand our reach to federally qualified health centers at a quicker rate. This would allow more data collection resulting in the establishment of a data set representative to populations that seek care at federally qualified health centers. In turn, this would allow the development of diagnostic data, predictive data, and finally prescriptive data. Further, funding would allow incorporation of additional technologies to ease data sharing. This includes health tracking devices, bluetooth devices used to measure health values, and potentially data sharing from applications used to track health parameters. In short, funding would allow for expansion and additional development.
In order to sustain cost over time, we plan to offer our program along with these additions to private clinics at a monthly rate. The uniqueness of our program is it’s versatility for tracking and meeting endless health goals along with its accessibility to all patients. With each step of this process we return to our mission which is to build long term relationships through accurate data tracking to implement preventative care through patient empowerment and adherence.
Stefan: Do you have any plans to make the dashboards accessible to the patients as well or are they exclusive to the clinics?
Amir: We will eventually add that feature to the program, but the data that patients would see will most likely be in a different format than what clinics see. Health literacy, accessibility, and education are factors that we need to consider when designing a platform for patients. The current goal is to build a user-friendly web application during the second phase of the project to give patients access to their data, provide real-time feedback and provide an additional platform for patients to communicate with their health care providers.
Stefan: What is the vision behind Pharmacists for Digital Health?
Emily: During our time in the Pharm.D. program, we are clinically trained to provide patient-centered care. What is understated and often overlooked is that data is everywhere, and even though our work as pharmacists may not be directly related to informatics or data science, the tools we use to practice - and really to live in this world - are powered by data in one way or another. Our goal with Pharmacists for Digital Health (PDH) is to merge this understanding with our clinical training and to gain enough proficiency to effectively find solutions in the inevitable and exciting junction between healthcare and the digital world.
Briton: What Emily and Amir have created is a space to help connect the dots between healthcare training and data science. Already, PDH has taken steps to honor the vision behind it.
Stefan: Thank you very much Amir, Briton, and Emily for this interview. We are looking forward to hearing more about the project in the future.
