In recent months, the public debate around artificial intelligence has often gravitated toward fears: job loss, algorithmic bias, dehumanisation of decision-making, and even dystopian futures of machines replacing humans and taking over the world.
These concerns are not entirely unfounded, and they deserve honest attention. But I believe we must simultaneously recognize a deeper and more urgent story: The transformative potential of AI and machine-learning technologies to advance health and medicine, to solve previously intractable problems, and to bring hope — especially in underserved and rural communities.
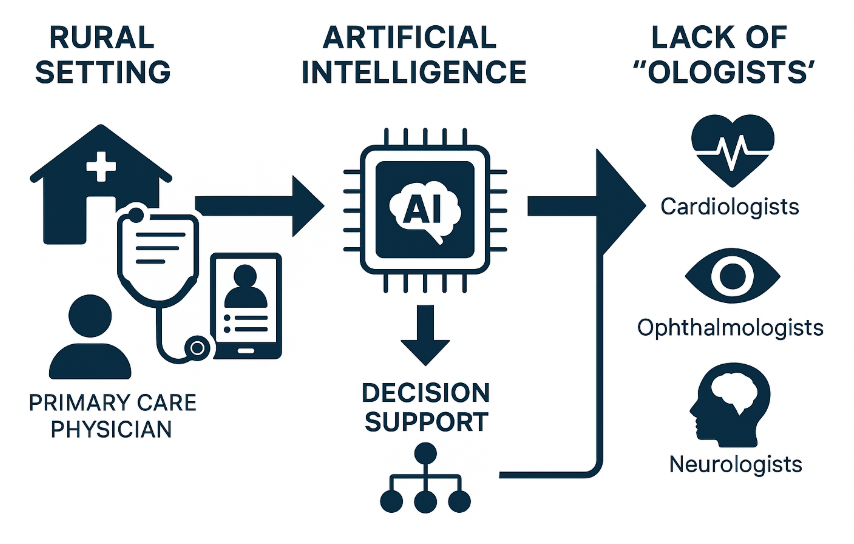
As the director of research at the Center for Health Systems Innovation (CHSI) at Oklahoma State University, I have been privileged to work with a talented team that is deploying predictive algorithms to address serious health problems in healthcare-deprived, rural settings (see see graphic below).
A recent article, Seeing the Future, published by OSU, detailed our work in developing a patent-pending AI-powered diabetic retinopathy risk-index system — based on millions of anonymized patient records — with the goal of helping primary-care physicians anticipate, intervene, and ultimately prevent irreversible vision loss. That work is a microcosm of what the broader field of AI in healthcare can, and should, accomplish.
“AI and machine learning have the potential to advance health and medicine, solve previously intractable problems, and bring hope — especially to rural and underserved communities.
The future of healthcare need not be one where robots and doctors stand opposed. I envision a future where AI becomes the digital stethoscope of rural clinics.” Dursun Delen, Director of Research at the Center for Health Systems Innovation
From fear to purpose
It is understandable that AI evokes anxiety. Too much of the media focuses on AI as replacing doctors, misdiagnosing patients, or entrenching inequities. But if we shift the narrative — from “machines replacing humans” to “machines empowering humans” — we open a far more constructive space.
AI should not be an abstract threat, but a tool, discipline-embedded and human-centered, deployed to amplify clinical insight, expand reach, and target the hardest healthcare problems.
One of the hardest problems is rural health-care disparity. In many rural settings, subspecialists are scarce, screening equipment is limited, and chronic diseases go undetected until severe. If you look at rural markets, we are significantly understaffed in primary care, and there’s almost a complete lack of subspecialists in rural markets. In that context, AI is not a luxury — it is a lifeline.
The promise for rural health equity
The mission of CHSI is to transform health and healthcare in rural and native American populations. The vast majority of our research projects focus on achieving this mission through advanced analytics and process optimization.
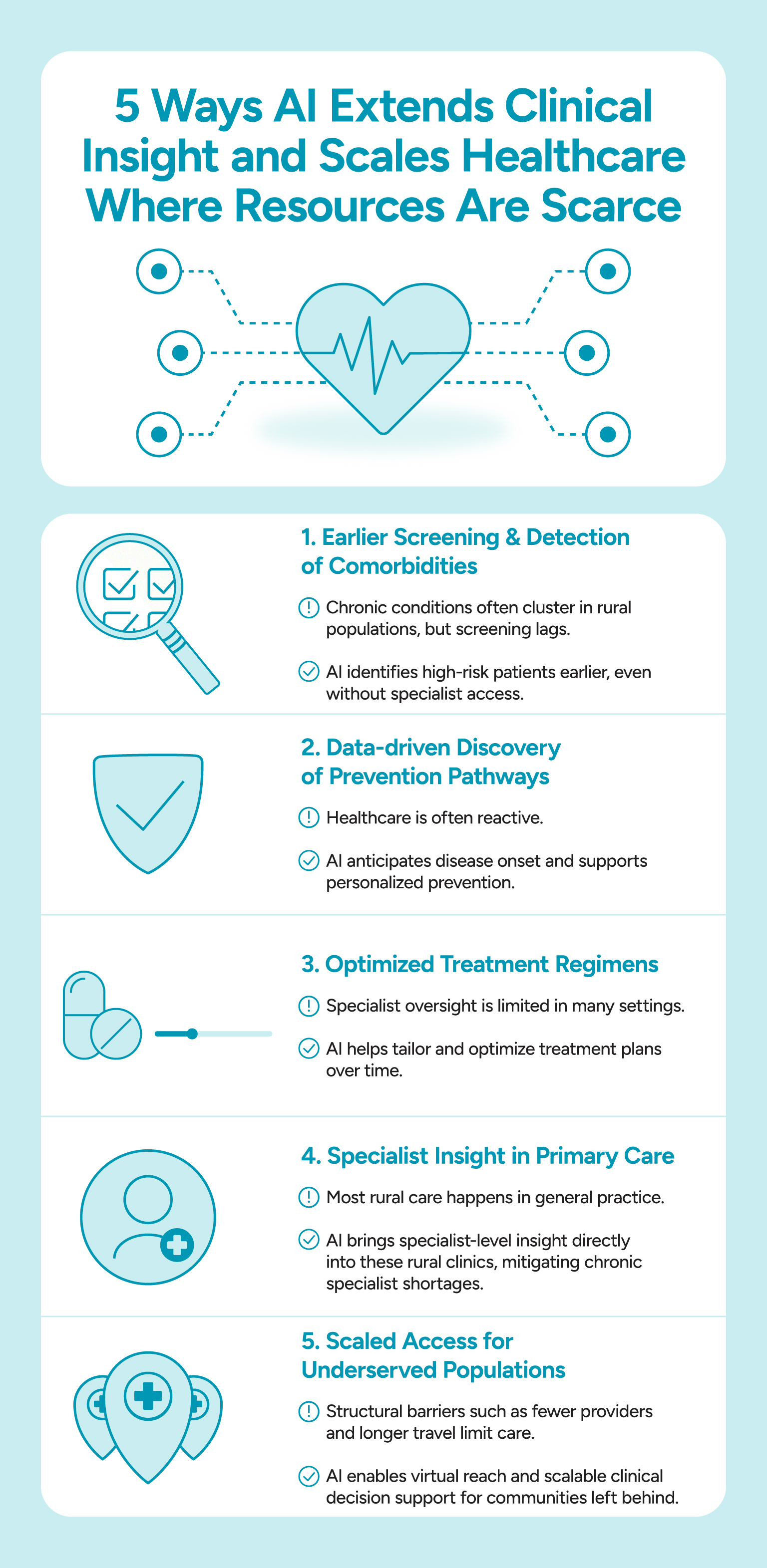
In this context, let me outline how AI can make a real difference in these underserved settings:
#1. Early screening and detection of comorbidities: Chronic diseases — diabetes, hypertension, chronic kidney disease, cardiovascular disease — often cluster in rural geographies, yet screening and follow‐up lag.
How AI helps: AI models trained on large datasets can help primary-care physicians identify high‐risk patients earlier, even when access to subspecialty care is minimal.
#2. Data-driven discovery of prevention pathways: Instead of just treating disease after it appears, we can become proactive:
How AI helps: AI can help flag patterns, suggest personalized risk-reduction strategies, and enable preventive medicine. The risk-index work at CHSI exemplifies that shift from reaction to anticipation.
#3. Optimized treatment regimens: Once disease is present, treatment plans are designed, but sometimes specialist oversight is limited. This is when AI can be especially powerful to optimize the regimens.
How AI helps: AI/ML (often in concert with operations research) can analyze rich clinical, imaging, and demographic data to tailor treatment, monitor response, and suggest optimizations.
#4. Deploying tools via primary‐care settings: In rural areas, the vast majority of care is delivered in general practice rather than large tertiary centers, where specialist insight is present.
How AI helps: AI tools embedded in the workflow of primary care — perhaps via decision-support dashboards, predictive alerts, or simplified screening modules — can extend specialist insight into rural clinics.
#5. Scaling access to underserved populations: The rural health disadvantage is often structural: fewer providers, longer travel, poorer infrastructure.
How AI helps: AI offers a way to scale decision-support, to provide “virtual subspecialty reach” into communities that otherwise would be left behind.
Why operations research + AI matters
At the recent 2025 INFORMS Annual Meeting — the flagship gathering of the field of operations research (OR) and analytics — one of the strongest thematic streams was on the use of AI/ML in healthcare and medicine.
Sessions such as “AI in Healthcare and Medical Research” underscored how OR/analytics frameworks are increasingly fused with AI techniques to address real-world clinical problems. These sessions emphasized not only predictive modeling, but also optimization, systems design, workflow integration, and equity. That synergy (between AI’s pattern-recognition and OR’s prescriptive decision-making frameworks) is precisely what we need if AI is to fulfil its promise in health-care settings.
Indeed, recent scholarship highlights this collaborative imperative. A 2025 report argues for research collaboration between AI and OR experts as a necessary step to maximize societal impact. In other words, the value is not simply in “building a better algorithm”, but in embedding it in a decision ecosystem that aligns with clinical workflows, ethics, resource constraints, and population-health goals.Addressing the concerns — and why they can be overcome
Of course, there are legitimate concerns: bias in training data, unequal access to infrastructure, the risk of “black-box” models replacing clinician judgment, and ethical issues around data privacy and trust. But rather than halt progress, these concerns should frame how we design and deploy AI systems:
- We must ensure data representativeness — rural patients, underserved populations, comorbidities prevalent in non-urban settings — so models don’t falter where they are needed most.
- We must integrate AI tools into provider workflows so they support rather than disrupt care, and preserve clinician autonomy.
- Governance and transparency must be baked in: explainable models, audit trails, clinician oversight.
- Implementation matters. A recent field guide for clinical AI shows that more than 80% of the work is not model engineering, but sociotechnical integration, data pipelines, economic and governance infrastructure. In rural settings, where infrastructure is more constrained, this implementation challenge looms large — but is exactly where we should invest.
The future of healthcare need not be one where robots and doctors stand opposed.
Instead, I envision a future where AI becomes the digital stethoscope of rural clinics, where predictive analytics become the standard of preventive medicine, and where underserved communities gain access to the same data-driven intelligence that once was the domain of elite academic centers.
As researchers, clinicians, and policymakers, our task is to pilot, validate, scale, and support those deployments with funding, workflow redesign, and training. At CHSI, we are demonstrating this in Oklahoma already through our diabetic retinopathy modelling and other projects. The theme at INFORMS — Smarter Decisions for a Better World — reminds us that technology is only part of the solution; the real goal is equitable, effective decision-making in health.
In summary, yes, AI carries risks — but it also carries hope. When deployed thoughtfully, in partnership with human clinicians, embedded in rural clinics, and aligned with operations-research perspectives, AI can help us move from managing disease to preventing it; from treating suffering to alleviating it; from underserved to equity. That is the future we should write.
Dursun Delen, Ph.D.
Regents Professor
Editor, Journal of Business Analytics
Spears Chair in Business Administration
Patterson Foundation Chair in Business Analytics
Director of Research, Center for Health Systems Innovation
Department of Management Science and Information Systems
Spears School of Business, Oklahoma State University
Phone: (918) 594-8283; Fax: (918) 594-8281
Email: dursun.delen@okstate.edu
Web: http://spears.okstate.edu/delen